Chronic Disease Outcomes From Primary Care Population Health Program Implementation
- Luisa Milton
- Mar 8, 2022
- 2 min read
Updated: Oct 3, 2024
Press Release:
In December 2017, The American Journal of Managed Care published a peer reviewed study which found that atients in practices with central population health coordinators had greater improvement in short-term chronic disease outcome measures compared with patients in practices without central support.
The study took place in the Massachusetts General Hospital Primary Care Practice-Based Research Network, consisting of 18 primary care practices. All practices in the network use electronic health records (EHRs) and have utilized a PHM health IT tool, TopCare, developed by SRG Technology for preventive cancer screening since 2011. In 2014, this PHM tool was expanded to include registries for patients with diabetes, cardiovascular disease (CVD), and hypertension (HTN). The tool identified network patients, assigned them to chronic disease registries, and tracked goal attainment in near real time. Researchers then developed a program for chronic disease management using central PHCs assigned to specific practices.
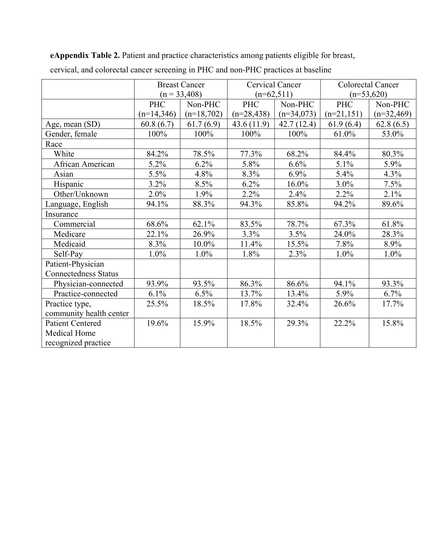
ABSTRACT Objectives: We implemented a health information technology—enabled population health management program for chronic disease management in academic hospital–affiliated primary care practices, then compared quality-of-care outcome measures among practices assigned a central population health coordinator (PHC) and those not assigned a PHC. Study Design: Quasi-experimental. Methods: Central PHCs were nonrandomly assigned to 8 of 18 practices. They met with physicians, managed lists of patients not at goal in chronic disease registries, and performed administrative tasks. In non-PHC practices, existing staff remained responsible for these tasks. The primary outcome was difference-in-differences over the 6-month follow-up period between PHC and non-PHC practices for outcome measures for diabetes (low-density lipoprotein cholesterol [LDL-C], glycated hemoglobin [A1C], and blood pressure [BP] goal attainment), cardiovascular disease (LDL-C goal attainment), and hypertension (BP goal attainment). Secondary outcomes included process measures only (obtaining LDL-C, A1C, and BP readings) and cancer screening test completion.
Results: The difference in the percentage point (PP) increase in outcome measures over follow-up was greater in PHC practices than non-PHC practices for all measures among patients with diabetes (LDL-C, 4.6 PP; A1C, 4.8 PP; BP, 4.7 PP), cardiovascular disease (LDL-C, 3.3 PP), and hypertension (BP, 2.3 PP) (adjusted P all <.001). Changes in cancer screening outcomes, which were not a focus of PHC efforts, were similar between PHC and non-PHC practices.
Conclusions: Use of central PHCs led to greater improvement in short-term chronic disease outcome measures compared with patients in practices not assigned a central PHC.
Am J Manag Care. 2017;23(12):728-735
























Comments